Strengthening the Health Professional Workforce
The Bipartisan Policy Center (BPC) recently released A Bipartisan Rx for Patient-Centered Care and System-Wide Cost Containment, an effort led by former Senators Tom Daschle, Bill Frist, Pete Domenici, and former OMB and CBO Director Dr. Alice Rivlin, that calls for a comprehensive approach to system-wide health care improvement and cost containment. As policymakers consider changes to federal health programs and the tax code, versions of many of the proposals included in our report have entered the national discussion. In a series of posts, we will provide a deeper dive into some of our proposals, along with comparisons to similar proposals, and, very importantly, how they fit into broader efforts for reform. Read the first, second, third, fourth and fifth entries in the series.
In a recent post, we discussed the potential benefits and risks associated with the move toward more coordinated and accountable systems of care. Collaboration, communication, and cooperation among providers and clinicians are essential elements of accountable care. A strong health professional workforce is needed to support high quality, value-driven care delivery and payment across the entire health care system.
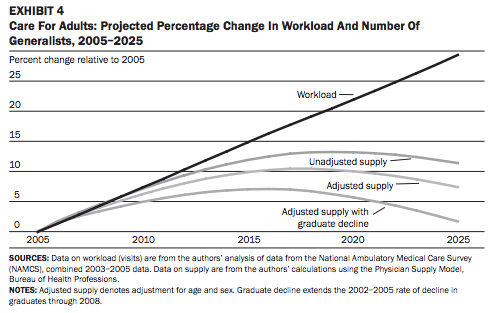
BPC’s health care cost containment report includes recommendations that would help strengthen our nation’s health care professional workforce. The report address two key concerns ? how to ensure we are leveraging opportunities to utilize the highest quality, most cost-effective professionals and how to ensure we have an adequate supply of primary care professionals to meet future needs. The report also includes recommendations to ensure that Medicare’s investment in Graduate Medical Education (GME) aligns with our overall vision for coordinated care, where providers are accountable for both cost and quality, in pursuit of a workforce that can most effectively and appropriately deliver care. Our GME recommendations will be detailed in a later post. The chart below illustrates projected demand for services (expressed as anticipated clinician workload) vs. the supply of generalist physicians over the next decade. The upcoming expansion of health insurance coverage to millions of Americans through implementation of the Affordable Care Act (ACA) has increased concerns that our nation will face a primary care provider shortage in the coming years.
Source: Colwill JM et al. Will Generalist Physician Supply Meet Demands Of An Increasing And Aging Population? Health Affairs 2008;27:w232-w241
BPC’s report supports greater utilization of non-physician professionals, such as advanced practice nurses (APNs) or physician assistants (PAs) to help meet growing primary care needs. For example, nurse practitioners (NPs), a type of APN, are able to perform many essential primary care services, such as taking patient histories, performing routine physical exams, and prescribing medications. According to the Institute of Medicine (IOM) 2010 report, The Future of Nursing: Leading Change, Advancing Health, “no studies suggest that APRNs are less able than physicians to deliver care that is safe, effective, and efficient or that care is better in states with more restrictive scope of practice regulations for APRNs.” Evidence shows that nurses consistently provide care that is on par with the quality of physician care on a number of different indicators.
Scope of practice laws, established by state law or regulation, determine how much flexibility APNs and PAs have to practice and bill independent of the oversight of a physician. These laws vary significantly across states. According to a recent paper released by the National Governors Association (NGA): 16 states and D.C. currently allow nurse practitioners full independence to practice at the top of their license, including diagnosis, treatment, referrals, and prescriptions; 8 states allow full independence with the exception of prescriptions; and 26 states require some level of physician involvement in NP practice, with ten of those 26 requiring a “collaborative” relationship with a physician for “consultation, referral, and review of provided care.”
State purview
The leaders of BPC’s Health Care Cost Containment Initiative believe that health professional licensure, and decisions about how best to structure collaborative or supervisory requirements for care delivery, should continue to be left to the states. BPC’s report calls for the elimination of outdated statutory or regulatory requirements in Medicare and Medicaid that interfere with states’ ability to regulate and determine scope of practice. This recommendation could have many different applications, but the report offers a specific illustrative example: Congress should strike language from the Medicare statute that requires physician “collaboration” as a condition of direct nurse practitioner reimbursement. This would ensure that in states where nurse practitioners already have flexibility to practice and bill independently, Medicare is not imposing additional, potentially complex or burdensome requirements for oversight. BPC’s report also recommends that the federal government offer states a financial incentive to broaden scope of practice for advanced practice nurses.
In alignment with IOM’s report, BPC’s report also supports state adoption of the National Council of State Boards of Nursing (NCSBN) advanced practice registered nurse model rules and regulations regarding scope of practice (Article XVIII). The NCSBN Model Act is the result of a collaborative effort among nursing organizations, state boards of nursing, educators and other stakeholders, and provides clarity and uniformity across a number of areas related to APN licensure, accreditation, certification, and education. However, rather than restricting nursing education funds to encourage states to adopt the NCSBN Model Act, as the IOM calls for, BPC’s report suggests providing an incentive for states that move forward with scope of practice. One possibility would be to forgive part of the Medicare Part D “clawback” ? in which states help fund drug assistance for low-income Medicare beneficiaries ? for states that adopt scope of practice policies that are no more restrictive than the Model Act. Approximately 17 states have adopted or are considering legislative and regulatory changes consistent with the NCSBN Model Act.
Role of the Federal Government
Activity at the federal level should focus on the removal of barriers to greater APN flexibility, consistent with state scope of practice requirements, and avoid conflicting standards that create confusion and administrative complexity for health professionals. BPC’s report recommends changes in federal statutes and regulations in order to support maximum flexibility for states, rather than imposing a federal mandate or pre-emption on health care professional scope of practice laws. It is important to note that the illustrative change to Medicare statute language above would not impact the ability of NPs to bill for services that are performed “incident to” physician care, such as seeing a patient to help carry out a treatment plan created by a physician. “Incident to” services are performed under the supervision of a physician and are reimbursed at 100 percent of the physician fee schedule. (Medicare reimburses NPs practicing independently, in collaboration with a physician, at 85 percent of the physician fee schedule). As the health care system moves toward more coordinated and integrated models of care delivery, relaxing scope of practice restrictions will allow teams of providers more flexibility to decide how best to divide up clinical responsibilities in service to patients.
BPC’s report also notes the importance of strategic investments to ensure an adequate supply of health professionals to meet future demand. The workforce funding in the ACA is largely discretionary, and thus it is highly vulnerable to ongoing budget battles and fiscal uncertainty. While BPC’s leaders are not advocating that Congress move forward with all the workforce programs authorized by the ACA, policymakers should be strategic about the best way to leverage limited financial resources. Defunding or disregarding a large number of these programs could result in missed opportunities to shore up the health care workforce, to provide support to vulnerable individuals with unique care needs, and to engage in strategic workforce planning at both the state and federal level.
Share
Read Next
Support Research Like This
With your support, BPC can continue to fund important research like this by combining the best ideas from both parties to promote health, security, and opportunity for all Americans.
Give NowRelated Articles
Join Our Mailing List
BPC drives principled and politically viable policy solutions through the power of rigorous analysis, painstaking negotiation, and aggressive advocacy.